Skyscapes
As David Stephenson’s Visions of Heaven: The Dome in European Architecture (New York: Princeton Architectural Press, 2005) reminds us, the Pantheon's oculus became one of the fundamental topoi of Christian and Islamic religious architecture from the fifth through the twentieth centuries. Glancing through Stephenson’s collection of medium-format photographs, one is reminded of one of those flip books which, if one turns fast enough, creates a miniature silent movie one can hold in one’s hand. In the establishing shot, the Pantheon's concrete appears bronzed and stained not just by the patina of age but by the water damage of two millenia, the orb of light burning a hole in the photographic plate. As the narrative unfolds, tastes in austerity and decoration ebb and flow in a calm rhythm, the pinhole at the center occupied now by the figure of Christ surrounded by the saints in the gilded mosaics of the early Christian basilicas, now giving way to a meditation in gray and white with an asymmetrical disposition of windows in the Church of the Ascension in Kolomenskoe, Russia. The impulse to decorate geometry reaches its peak in the domes of the Renaissance, my favorite of which is the eleventh-century Duomo in Parma, to which sixteenth-century frescoes by Carregio were added in which there is a figure tumbling through the aperture surrounded by a host of angels struggling for position amongst the billowing clouds. The Renaissance knew severity and introspection, too, as a string of pared-down domes such as the Duomo in Padua and San Salvatore and San Giorgio Maggiore, both in Venice, attest. In Antonio Galli Babiena’s Santa Maria Assumpta in Sabbionnetta, one of the planned Renaissance towns, the view of the sky reaches frank theatrical illusionism as a trompe l'oeil painted onto the dome behind a latticework screen. Since the sky is everywhere, the hole at the center is now occupied by a dove. There are tropical palms in the seventeenth-century Dom St. Jakob in
The Pantheon, built by Hadrian in 138

San Lorenzo, in Turin, 1668-87, Guarino Guarini

From David Stephenson's Dome Series
The minimalist James Turrell has spoken of an interest in public spaces so ancient that they have come to be emptied of their meanings, like Nietzsche’s coins. One of his favourite buildings is the Pantheon, of which his Skyspaces are direct descendents. Strewn across locations as far flung as Santa Fe,
Nowhere is this architectonics of the heavens more evident than in Turrell’s Live Oak Friends Meeting Hall in
Live Oak Friends Meeting Hall, Houston, TX

Atget's Dead Spaces
Atget’s streets are famously emptied of people–-he gives the sense of Paris as an abandoned city. Perhaps the founder of the anthropological gesture in photography, he documented the existence of human beings from the material traces they left behind. As John Szarkowski puts it, “it might have been that Atget found the things that people make more interesting than their makers." Still, when one looks closely, there are plenty of people in Atget’s photographs, only a few of whom have been able to stand still long enough to be captured posing in a proprietary fashion at the door of an establishment or standing in conversation at a street corner. There were countless others either unable or unwilling to demonstrate the degree of endurance required by his camera, so that they appear only as ghostly blurs. In one of his photographs, “Rue Cherubini,” taken in 1907, there is a solitary man in a butcher's apron who turns out on closer examination to be part of a larger group, several of whom must have moved during the recording of the image so that they appear if not like cherubs then at least like birds who have taken flight. It may be this that lends Atget's photographs the tranquility spoken of by Walter Benjamin.
Atget had the now rather banal insight that photography, at least before the invention of color, was most effective as a meditation on texture: his photographs often feature swathes of leaves or ivy, walls of brick and flights of stairs or cobblestone streets - most famously in Les Halles, but in every other arondissement of the city as well. His sense of humor is most evident in his fondness for repetition, which could be said ultimately to stem from this appreciation for texture, as seen in the carcasses of meat (also at Les Halles), the chairs of a café, or the famous corsets and empty suits published in La Révolution surréaliste, in which Benjamin (whose version of Atget was largely that of the Surrealists) discerned the destruction of the aura
Thirty-nine plates of Atget’s photographs of trees in the gardens of Saint-Cloud were recently rediscovered in the archives of the Bibliothèque Nationale (Eugène Atget’s Trees,
In another image, a gnarled root is viewed from below as it climbs down a hillside, entirely occupying the left side of the photograph, while an expanse of white light burns out the right. Ultimately, we arrive at a group in which the gnarled roots and leaves blanketing the ground have become more important than the now greatly truncated tree. Guillaume Le Gall points out how Atget’s practice in these photographs continues his lifelong indifference to the pictorialist aesthetic that dominated the art photography of his day. In a treatise on the proper depiction of trees, Robert Karl insisted that the foreground must be executed with a restraint and discernment characteristic of painting or drawing, never falling prey to the temptations of exaggerated foreshortening offered by the low-angle perspective of the camera lens: “There is good reason to deliberately reduce the foreground’s proportion. If one followed this proportion strictly, the overall view would noticeably diminish in size and extent, as the foreground, particularly if it is made up of tree trunks, would hide a large part of the landscape.” This is exactly what has happened in Atget’s photographs of tree roots, in which the foreground has become the posed subject of the image.
Similarly, while Atget's photographs often have a strong sense of depth defined by a vanishing point tucked in amongst a well of houses or located just around the corner of a long and winding street, they seem just as often to pull the viewer up short against an object that has been placed in the center of the composition, such as a doorway or a fountain, a column or a pedestal, even the bed of an upturned handcart. He had a tendency to place large dead objects at the center of his images, often trees--as in this photograph, in which the blank foreground of a reflecting pond has been obscured by a tree trunk:

This late photograph of Notre Dame, taken in 1925, demonstrates that Benjamin was right to qualify his remark that "Atget almost always passed by the 'great sights and so-called landmarks.'" One might say that this photograph enacts less a destruction than an interruption of the aura. It also demonstrates that Atget's enemy was not the ancient Paris of the kings, but the bourgeois city of Haussmann's boulevards, on which he turned his back.

The Waggle Dance

These Insects lived like Men, and all
Our Actions they perform’d in small:
They did whatever’s done in Town,
And what belongs to Sword, or Gown:
Tho’ th’Artful Works, by nimble Slight
Of minute Limbs, ‘scaped Human Sight;
Yet we’ve no Engines, Laborers,
Ships, Castles, Arms, Artificers,
Craft, Science, Shop, or Instrument;
But they had an Equivalent;
Which, since their Language is unknown,
Must be call’d, as we do our own.
―Mandeville, The Fable of the Bees
Apis mellifera, the European honeybee, lives in hives of up to 40,000 bees. The social order of the hive is well known to every elementary school student, consisting of a queen bee, a few male drones whose task it is to fertilize the queen, and thousands of infertile females who serve as worker bees. There is an additional division of labor among the workers, some of whom build the hive, while others maintain it, and still others forage for food and tend to the young. Nectar is the honey bee's primary food source and occurs throughout the territory around the hive in patches that are larger than a single bee can harvest. When a scout bee discovers such a patch, she flies back to the hive in order to recruit the other workers, a task she accomplishes by performing what the Austrian ethologist Karl von Frisch has termed the "waggle dance." The dance consists of a figure of eight with two signifying components: a straight line, the angle of which communicates the direction in relation to the angle of the sun in which the other bees need to fly in order to find food, and the speed of the waggle, which indicates its distance from the hive. The scout can adjust the angle of the dance the longer she remains in the hive so that it corresponds to the direction in which the sun is moving across the sky, thus incorporating an element of time. Finally, she provides the other bees with a sample of the nectar, the odor of which has been demonstrated in experiments to be essential to their success in finding the patch. Space and time are both implied in the dance language of the honey bee, but it remains grounded in sensuous knowledge.
Von Frisch received the Nobel Prize in Physiology and Medicine along with fellow ethologists Konrad Lorenz and Nikolaas Tinbergen in 1973 for his work on the dance language of the honey bee and other aspects of insect communication. At the time, his theory was disputed by the American biologist Adrian Wenner, although it has since been confirmed and expanded by the research of James L. Gould. Although the field of ethology aims to keep the study of animal behavior free of human analogy, the centrality of the classical problem of the origin of language remains evident in von Frisch's work. In turn, his theory of bee communication has proven applicable to human organizational models such as the 'bee colony optimization' used to design Internet servers. Boasting of the perfect analogy between the hive and human society, Mandeville captures the problem nicely when he concedes that the unknown character of animal language forces even the most rigorously descriptive of sciences to conceptualize it in human terms. The acknowledgment of this unknowability, however fleeting, interrupts the circularity of the analogy and begins to separate science (in this case social science) from metaphor. At the same time, it becomes reincorporated into the system as the even more contemporary acknowledgment that the break will never be clean.
Napoleon of the Neuroses
The founder of modern neurology, Charcot became a resident doctor at the Salpêtrière, a Parisian hospice for indigent patients, in 1862 and founded its neurology clinic in 1882, becoming the first professor of neurology in the same year. Among the diseases he described that still belong to the nosological apparatus of contemporary neurologists were multiple sclerosis; amyotrophic lateral sclerosis, initially dubbed Charcot’s disease, only later Lou Gehrig’s disease; Charcot-Marie-Tooth disease, a hereditary neuropathy of the legs and feet now thought to be associated with changes in the myelin gene PMP-22; and Charcot joint, a progressive degeneration of the foot joints as a result of peripheral neuropathy, associated with syphilis in Charcot’s day, diabetes in our own. He was also involved in the elucidation of two neurological disorders, Parkinson’s disease and Tourette’s syndrome, that he proposed be named after his students, demonstrating the importance of the small arteries in cerebral hemorrhage as well as making important discoveries concerning the mechanisms of peripheral arterial disease such as intermittent claudication that can lead to gangrene and amputation. Among his discoveries outside of the realm of neurology were Charcot's triad, the combination of fever, jaundice and upper abdominal pain associated with infection of the common bile duct most often the result of gallstones; and Charcot-Leyden crystals, the needle-shaped phosphate crystals still considered a characteristic pathological finding in asthma. As Joseph Babinski once put it, “to take away from neurology all the discoveries made by Charcot would be to render it unrecognizable.”
Charcot was one of the virtuoso practitioners of nineteenth-century empiricism and positivism. Before he became a professor of neurology, he was a professor of anatomical pathology, deploying the “clinical-anatomical method” developed by the seventeenth-century Italian pathologist Giovanni Morgagni and refined by the French clinician Rene Laennec to correlate the clinical symptoms observed in patients with anatomic lesions discovered at the time of autopsy. He was among the founders of the discipline of neuroanatomy that remains the central to the methods of neuroscience. For all its fruitfulness, however, Charcot’s method required no major technological innovation: the basic methods of gross anatomical pathology he employed in the elucidation of neurological disorders were already in place by the eighteenth century, and Virchow developed the field of microscopic pathology earlier in the nineteenth. Even Charcot’s interest in photography was adopted from his mentor, Guillaume Duchenne, who also bequeathed to him a large collection of anatomical specimens. Indeed, it was Charcot’s attempts to expand his methods to experiment with the new paramedical technologies of his day, most notably electromagnetism, as well as his willingness to take advantage of his flair for the theatrical that caused the greatest damage to his reputation.
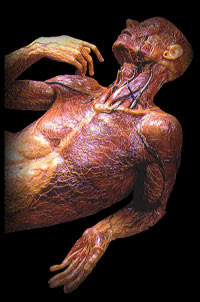
Eighteenth-century anatomical wax model in Museo La Specola, Florence. By this period, the methods of gross pathology were already in place.
Known to the fashionable crowds who gathered to see his Tuesday lectures as the “Napoleon of the Neuroses” and the “Caesar of the Salpêtrière,” Charcot has sometimes also been credited as the founder of psychopathology. His primary contribution to this field was his revival of the diagnosis of hysteria, which he regarded not as a form of malingering (as it had come to be regarded), but as a hereditary neurological disorder, focusing on neurological symptoms such as motor paralysis, sensory loss, convulsions and amnesia in an effort echoed in the desire of contemporary neurologists to treat conversion and catatonia primarily as movement disorders. Similarly, Charcot constructed maps of what he termed "hysterogenic zones" that are strikingly similar to contemporary diagrams of fibromyalgia points. While he was unable to associate hysteria with any anatomical lesion, acknowledging that it was what would nowadays be termed a functional disorder that could not be accounted for within the parameters of the clinico-anatomical method, he performed careful clinical experiments that demonstrated the physiological differences between hysteria, the muscular contractures of which he observed to be smooth with unlabored respiration, and malingering, in which such contractures were accompanied by muscle fatigue and progressively labored breathing. As Freud famously put it, Charcot threw “the whole weight of his authority on the side of the genuineness and objectivity of hysterical phenomena," defending the hysteric against charges that she was a fake. William James concurred, observing that "amongst all the many victims of medical ignorance clad in authority, the poor hysteric has hitherto fared the worst; and her gradual rehabilitation and rescue will count among the philanthropic conquests of our generation." The feminist psychiatrist Judith Herman points out the paternalistic nature of this effort, observing that, while the feminist movement was relatively weak during the

Contemporary diagram of fibromyalgia points.
Although he continued to give the “nomadic uterus” and its fixation by what seem now like barbaric methods such as the uterine compression belt a central role in the treatment of hysteria, Charcot was also famous for his insistence that hysteria was by no means specific to the female sex. Regarding male hysteria as underdiagnosed, he maintained that it was "not at all rare," occurring in men of all ages and social classes, even in those “without an effeminate exterior,” and relating it to traumas including railroad accidents and industrial work injuries. He saw the clinical presentation of male hysteria as similar to, although less dynamic than, the female version, with a greater incidence of static symptoms such as hemianesthesia, tunnel vision and muscular contractures. "Little by little," he told his students, "you will acquire the habit of speaking of hysteria in men without thinking in any way of the uterus." Charcot thus did a great deal to establish a diagnosis that was to become extremely important with the appearance of shell shock during World War I, becoming the object of study of psychologists as diverse as William Rivers and Freud and ultimately featuring prominently in Walter Benjamin’s diagnosis of the literature of modernity in poets such as Baudelaire.

Douglas Gordon, "10ms-1," 1994, a video installation looping footage of a WWI soldier with shell shock on an infinite repeat
The neurologist Christopher Goetz has proposed that “in attempting to impose on hysteria the clinicoanatomic strategy he had used previously with success, [Charcot] faltered." It would perhaps be more accurate to say that Charcot was forced in the case of hysteria to depart from the clinico-anatomical method -- with scandalous results. Goetz maintains that Charcot's work on hysteria can be divided into two phases, a descriptive phase prior to 1877 in which he was concerned to categorize the symptoms and isolate the patterns and phases of the disorder, and an etiological phase after 1877, in which he initiated his experiments in the auditorium. In the first phase, he worked with the graphic illustrator Paul Richer, seated at the table in Brouillet's iconic 1887 painting "A Clinical Lesson at the Salpêtrière" (a lithograph of which Freud kept in his study throughout his career) and later professor of artistic anatomy at the Ecole des Beaux-Arts, to use medical illustration as a means of delineating the clinical features of hysteria, a project he later amplified with the use of photography under the direction of Albert Londe, the medical photographer of the Salpêtrière who was to become an expert in x-ray photography. In the second phase, Charcot developed the hypnotic experiments that he conducted in his amphitheatre before the eyes of an admiring public, noting that hysterical contractures could be removed if a patient passed into a lethargic state and made to persist if she became cataleptic. [One of Charcot's fundamental tenets was thus the linkage of hysteria and hypnotism, an emphasis on the role of suggestion that became the basis for his prolonged and bitter disagreement with Charles Bernheim.]
At the Salpêtrière, Charcot discovered the existence of a new disorder that was not to be named after him, but which he termed “hystero-epilepsy," also known as "la grande hystérie." Charcot worked to characterize the phases of the hysteroepileptic attack, an account of which is found in his 1887 treatise authored with Richer, Les Démoniaques dans l’art. In his description, the attack began with an prodrome that often appeared several days in advance, including loss of appetite and vomiting, in which the patient became taciturn and melancholic or suffered from overexcitation. It was sometimes accompanied by visual hallucinations, including visions of animals, cramps or trembling of the limbs and a jerking of the body along with vertigo. Immediately before the attack, there was an hysterical aura followed by loss of consciousness as the attack proper began, divided into four phases. The initial epileptoid phase mimicked a seizure and could, Charcot remarked, be “mistaken” for one, lasting 1-3 mins. and consisting of three phases. The tonic phase was described as starting with a momentary arrest of inspiration, with pallor followed by flushing and facial distortion, sometimes protrusion of the tongue. It ended with a tetanous immobilization of the body that frequently involved extension of the trunk and limbs, followed by in the clonic phase, a large generalized seizure accompanied by dreadful grimacing. This was followed by the phase of resolution, in which the face was xx, the eyes closed, and the muscles completely relaxed. These initial phases lasted about a minute each, the resolution phase 2-3 minutes.
The second phase of the attack was described as the “period of clownism.” After a moment of calm, it was characterized by contorsions and “grand movements,” phenomena that Charcot saw as linked by a principle he termed “an exaggerated discharge of muscular force.” It was in this phase that the famous arc-en-cercle, or arching of the back, occurred. In this phase, the patient was capable of displaying “a suppleness and agility, a muscular strength that may astonish the spectator.” With a delicate discernment of gender differences, Charcot noted that women might greatly exceed the physical strength expected of their age and sex, whereas “in men, this period sometimes achieves a degree of violence that exceeds anything one can imagine.” It was this phase that Charcot linked to the demoniacal possession of religious ecstasy examined in Les Demoniaques dans l'art. The third phase was described as a phase of "plastic poses" or what he termed "passionate attitudes" [attitudes passionelles], lasting from 5-15 mins. in which the patient displayed happy, sad or frightened affect and frequently spoke or shouted. In the terminal phase, similar to the epileptic's post-ictal state, the patient partially regained consciousness, but might remain delirious for periods of up to an hour.



As Goetz points out, Charcot never liked the term "hystero-epilepsy," with its implication that hysteria could be classified as a form of epilepsy. Although he noted that the hystero-epileptic attack resembled true epilepsy, and also that the latter sometimes occurred in conjunction with hysteria, he regarded the two disorders as distinct. "We are dealing always and exclusively with hysteria," he declared, "but hysteria taking on the appearance of epilepsy" (italics mine). Hystero-epilepsy was not a separate diagnosis, but one of many possible manifestations of hysteria. "It is likely that hysteria in the guise of epilepsy is only an exaggerated form," he insisted, "the highest development of this tonic variety of ordinary hysteria."
While Goetz defends Charcot's early descriptive work, Georges Didi-Huberman has observed that there was far more than description at stake in Charcot's classification of the phases of the hysteroepileptic attack. "Charcot's 'genius,'" Didi-Huberman proposes, was "not simply to arrive at a description...but to calibrate it into a general type that can be called 'the great hysterical attack.'" He argues that Charcot imposed on hysteria a form and regularity required by the epistemological dictates of rationalist positivism, the goal of which was the production of an hysterical "type." "Charcot domesticated the most Baroque theatricality," argues Didi-Huberman, "he achieved the coup de force, and I mean force, of making theatricality into not only a clinical, but a classical tableau...Charcot was a kind of entrepreneur and sponsor of the narrative and iconic type required by the principles of his concept of hysteria and his epistemological objectives…constraining the real to resemble the rational." For Didi-Huberman, Charcot’s efforts to provide a medical account of hysteria are thus both a domestication and the imposition of a particular genre, namely that of the classical tableau, a forerunner of photography in which actors were arranged in poses in order to reenact scenes from famous paintings. First enacting a “dramaturgical cutting of … symptoms into acts, scenes, and tableaux," Charcot's rationalism thus required an additional reduction of the theatrical and dynamic to the painterly and static. As an art historian, he emphasizes the graphic dimensions of Charcot's project, observing that Charcot's method was "primarily visual" and pointing out the role that the illustrator Paul Richer played in the production of the regular forms of the classic hystero-epileptic attack, sketching eighty-six poses that were later whittled down to nine and organizing them into a chart that offered a schematic overview of the onset and development of the attack. For Didi-Huberman, this chart became the "figurative standard" for Charcot's conception of hystero-epilepsy. Once the standard had been established, it remained only to fit the patient into it. Didi-Huberman thus characterizes Charcot's most famous patient, Augustine, who became the photographic model for most of the series of photographs published in the first Iconographie photographique de la Salpêtrière, as the “’most classical’ example of the model,” since the temporal progression of her attacks conformed almost perfectly to the clearly delineated phases of Richer's illustrations. Placed by the camera into the static poses of the tableau, Augustine thus met the demands of Charcot's typology. She was Charcot's "masterpiece," "the star model for a whole concept of hysteria."

Charcot's most famous patient, Augustine, pictured in her "normal state" and during an hysterical contracture. Ulrich Baer has referred to the latter photograph as an example of "pseudo-medical pornography."

Augustine during the emotional phase of an hysterico-epileptic attack
In Les Demoniaques dans l’art, Charcot boasts that he has “been able to give the great hysterical attack a methodical description and to subdivide it into numerous phases and periods that have been neatly characterized. Where authors have only seen disorder and confusion, we have shown the existence of an immutable and fixed rule around a type that represents the hysterical attack in its entire and complete development, and we have grouped the varieties resulting from the predominance or attenuation of one of the several periods that compose it.” Emphasizing the precision of his delineation of the phases of hysteroepilepsy, Charcot boasts of the methodical and organized character of his description, which has led to the discernment of the fixed and immutable rules of the natural world in place of meaningless disorder and confusion. The effect is to produce a typology held to be entire and complete and into which varieties and subtypes of the disorder may be classified based on the predominance of one or another of the key phases. While the description is thus timeless and totalizing, Charcot notes proudly that it “will be as succinct as possible,” observing that “for clarity and ease, we will introduce a number of figures that illustrate [our] special work on the question.” As Didi-Huberman observes, Richer's figures thus occupy a crucial position in the construction of the typology, allowing it to attain an ease and concision not attainable by words alone. The figures accompany and, in the layout of the text, even precede the verbal description, anticipating and in a sense ultimately short-circuiting it.

Paul Richer's illustration of the arc-en-cercle

Louise Bourgeois, Arch of Hysteria, 1993
In the end, it was hysterico-epilepsy that led the Napoleon of the Neuroses to his
Ultimately, Charcot accepted Babinski's critique, the two collaborating to devise a treatment that combined counter-suggestion, with the staff withdrawing all interest in the hysteric's epileptic symptoms, and isolation, sending the hysteric back to the general ward away from the epileptics. The results of this treatment in terms of the resolution of epileptic symptoms were said to be impressive. Still, the damage had been done: the showmanship of Charcot’s Tuesday lectures was vilified in Axel Munthe’s scathing attack on his time at the Salpêtrière, and the great neurologist's reputation with Parisian society never fully recovered. In the end, Charcot is said to have regretted his work on hystero-epilepsy. A few days before his death, he was reported to have conceded that "our conception of hysteria has become obsolete. A total revamping of this area of neurologic disease is required." Apparently, he particularly regretted his role in the popularization of hypnotism and his interest in paramedical technologies such as magnets, electricity and metals.

Andre Brouillet's 1887 Salon painting, "A Clinical Lesson at the Salpêtrière." Babinski holds up the patient, and Paul Richer (Charcot's medical illustrator) sits at the table. Other pupils of Charcot, including de la Tourette, Raymond, Brissaud, Joffroy, Bourneville and Ballet, are depicted in the audience.
This version of Charcot's career is reiterated in influential histories of psychiatry and psychoanalysis such as Henri Ellenberger’s The Discovery of the Unconscious. The basic elements of Babinski’s and Munthe’s critique are also adopted in Didi-Huberman’s Invention of Hysteria. (see also Baer) Indeed, it is common among the media theorists who have focused on the visual regimes governing Charcot’s conception of hysteria to assume that he “invented” a disorder that no longer exists. Friedrich Kittler, for example, observes that "the 'great hysterical arc' can no longer be found in the lecture halls of today's medical schools," arguing that Charcot’s hystero-epilepsy should be understood as an effect of filmic technologies that "disappears from nosology of the world shortly after its storage on film.”
By comparison, psychiatrists continue to believe that what Charcot termed hysteria continues to exist. Guillain, a biographer of Charcot who served as a psychiatrist at the Salpêtrière in the 1960's, compared the percentage of cases diagnosed as hysteria by Charcot with those he himself later diagnosed at the same institution, finding that "the patients have not changed since Charcot's times, but the terminology applied to them has." While one well-known study has shown that the misdiagnosis of conversion disorder has decreased since the dramatic advances in neurology's use of diagnostic imaging (with 50% of cases initially diagnosed as conversion in 1965 later found to have neurological disease, whereas misdiagnosis is now thought to constitute between 4 and 10% of cases), it is still estimated to constitute 1-4% of diagnoses in Western hospitals. "The symptoms themselves have never changed," Patrik Veilleumier, a neurologist at the
Neither the media historians nor the psychiatrists appear entirely correct. While hysteria was not the invention of Charcot’s nineteenth-century positivism and it did not disappear with decline of filmic technologies for the recording of clinical presentations, hysteria has been changed by its contemporary incarnation as conversion disorder. In what follows, I will attempt to examine the evolution in the visual economies of hysteria that has occurred between Charcot and the present day.
In the DSM-III in 1980, psychogenic conversion was definitively stripped of all association with the uterus when "hysterical neurosis, conversion type," was renamed "conversion disorder," now defined as the production of quasi-neurologic symptoms such as blindness, paralysis and seizure. In the New York Times, William E. Narrow, associate director of the research division of the American Psychiatric Association, remarked that "hysteria, to me, has always been a pejorative term, because of its association with women. I think the fact we got rid of that word is a good thing." He could, perhaps, have been more precise, since the word he presumably meant to 'get rid of' was the uterus, never more than a metonymy for woman as such, and really more the etiological misattribution of a symptom to an unsubstantiated underlying anatomical defect. Ultimately, the new nomenclature was the culmination of Charcot's insistence that his students "should acquire the habit of speaking of hysteria ... without thinking in any way of the uterus." Indeed, the contemporary criteria for conversion disorder enumerated in DSM-IV bear such remarkable similarities to Charcot's view that one might argue that they constitute a re-neurologization of hysteria, the ultimate effect of which is the elision of any psychoanalytic explanation of hysterical symptoms on the level of unconscious desire.
The most basic criteria for the diagnosis of conversion disorder is the presence of "one or more symptoms or deficits affecting voluntary motor or sensory functioning that suggest a neurological or other general medical condition." As with many diagnoses in the DSM, conversion disorder requires that the symptom not be "fully" (the term is generally "better") explained 'by a general medical condition or as the direct effects of a substance,' thus acknowledging that conversion, while it suggests a neurological condition, lacks an organic lesion and thus eludes the clinico-anatomic method still encapsulated in the neurologist's demand to "localize the lesion." Considerable care is nonetheless taken to differentiate conversion from two DSM diagnoses characterized by the voluntary production of somatic symptoms, namely malingering (in which both the production and the motivation of symptoms are voluntary) and, more subtly, factitious disorder (in which the production of the symptoms may be voluntary, but their motivation remains obscure to the patient and occurs on the level of primary gain). Medical science thus remains torn between continuing to defend the hysteric's honor against charges of faking and the more troubling realization that conversion continues, whatever the patient's intention may be, to present the false appearance of a neurological disorder. Conversion has still not been rid of its dangerous capacity for representation-as-dissimulation and, worse still, for making a fool of the physician.
The second major criterion, which falls short of offering an etiological account of conversion, is the judgment that psychological factors are present since 'the initiation or exacerbation of the symptom or deficit is preceded by conflicts or other stressors.' Charcot's patient Augustine, who maintained, like many other female hysterics in the Salpêtrière, that she had been raped (in her case by her employer at razor point at the age of 13), would fit both criteria, since her seizures were both manifestly neurological in appearance and had a psychological stressor as their immediate precipitant: "A few days [after the rape and the subsequent onset of bleeding, mistaken for her first menses], [she] was lying in her room and became frightened when she saw the green eyes of a cat looking at her; when she cried out, her mother arrived to find her utterly terrified and bleeding from her nose. Then the attacks broke out..." The basic phenomena that interested Charcot (motor contractures, opthalmological symptoms, and the notorious hystero-epilepsy) remain largely unchanged in the four subtypes of conversion disorder, 'with motor symptom or deficit,' 'with sensory symptom or deficit,' 'with seizures or convulsions' (with which Augustine would presumably have been diagnosed) and 'with mixed presentation.' Perhaps the major departure is the stipulation that the symptom cannot be explained 'as a culturally sanctioned behavior or experience,' a common gesture in the DSM that in this case serves to exclude the intimate association between hysteria and female religious experience that interested Charcot so much.

Interestingly, the misdiagnosis of conversion disorder is thought to have decreased since the dramatic advances in neurology's use of diagnostic imaging tools: in 1965, 50% of cases initially diagnosed as conversion were later found to have neurological disease, whereas misdiagnosis is now thought to constitute between 4 and 10% of cases. It is estimated to constitute 1-4% of diagnoses in Western hospitals. Goetz observes that Guillain, a biographer of Charcot who served as a psychiatrist at the Salpêtrière in the 1960's, compared the percentage of cases diagnosed as hysteria by Charcot with those "he himself diagnosed at the same institution over a comparable period in our century," finding that "the patients have not changed since Charcot's times, but the terminology applied to them has." "The symptoms themselves have never changed," Patrik Veilleumier, a neurologist at the
So what has become of what Charcot termed hystero-epilepsy? It, too, survives largely intact as the disorder currently known as PNES, or "psychogenic non-epileptic seizures." Once again, a fair amount of ideological position-taking is wrapped up in a name. Thus, from a summary of the literature on PNES for use by clinicians: "the terms 'hysterical' seizure or 'hysteroepilepsy' are now discouraged as both pejorative and oversimplified, failing to capture the broad range of psychopathology ... The term 'pseudoseizures' is also discouraged, since the root 'pseudo' or false invalidates the genuine, even if psychogenic, disorder that a patient experiences." As with conversion disorder, any reference to the uterus is to be avoided as much because it is regarded as disparaging or belittling as because it has been shown to be inaccurate, although in this case a concern is also expressed that it implies a single etiology that belies the considerable variety of underlying psychopathology. The term 'pseudoseizures' is similarly problematic because it implies that psychogenic seizures are disingenuous, thus perpetuating the clinician's chivalrous defense of the hysterical patient's honor. Still, the word 'mimicry' continues to feature prominently in the definition of psychogenic seizures, defined as "events that clinically mimic epileptic seizures but are not associated with physiological CNS dysfunction and are instead psychogenically determined." PNES thus constitutes a case of genuine mimicry, which is to say that it moves the production of mimetic symptoms onto the level of the unconscious (or, in the more neutral language of neurology, the involuntary) without denying that the nature of these symptoms is the production of false appearances.
While the patient's intention thus represents a crucial moral issue in the diagnosis of PNES, the production of false appearances continues to constitute the central challenge for the neurologist, whose primary goal is to accurately differentiate between psychogenic and epileptic seizures. The costs of missing a diagnosis of PNES are presented primarily in terms of the dangers of unnecessary treatment with antiepileptics, with the associated risk of drug toxicity, a consideration that is not insignificant given the association of these drugs with major side-effects such as congenital birth defects and Stevens-Johnson syndrome. The concern is presented as especially serious in the case of the psychogenic production of status epilepticus (seizures lasting more than 30 minutes), in which protocols call for the administration of toxic levels of antiepileptics as well as invasive procedures such as intubation and iatrogenically-induced coma. This may be a particularly significant consideration since one of the characteristics of psychogenic seizures is that they tend to be of longer duration than epileptic seizures, which typically last less than a minute. It is also pointed out that anti-epileptics administered during pregnancy carry significant risk of birth defects, a particularly relevant issue given that the female predominance of PNES is estimated to be between 65 and 90%, with the most common onset in the third decade of life, i.e. during the child-bearing years. Still, one wonders whether the increasingly widespread use of antiepileptics by psychiatrists for their mood stabilization properties reduces the force of this objection. In the rather chilling language of medical cost-benefit analysis, an additional reason given for the need for an accurate diagnosis is that it precludes unnecessary ER visits and hospitalizations, which "place a cost burden on the healthcare system." How great the societal burden of hysteria really is or how it compares, for example, to the use of xx remains unexplored. Finally, it is stated that an accurate diagnosis is required in order for the patient to receive necessary psychiatric treatment, despite the fact that the results of such treatments (which include individual psychotherapy, group therapy, and family education) are acknowledged to be mixed, none holding out hope for a reliable resolution of symptoms.
Such concerns are reiterated in the context of the common procedure of provoking seizures in patients who do not produce them spontaneously when admitted on an inpatient basis for EEG monitoring, the gold standard both for the diagnosis of epileptic seizures and for their differentiation from PNES. When PNES is suspected, this is frequently done by administering a placebo in the form of IV saline or rubbing alcohol on the skin. Indicating the special power of suggestion in psychogenic seizures, "67-90% of patients with [this disorder] will have a typical event" when informed that such treatments are likely to produce an episode, whereas the occurrence of epileptic events is considerably lower. "While facilitating diagnosis, the inherent deceit in this approach may jeopardize the physician-patient relationship and impede future treatment efforts," the authors concede. "However, many experts believe that these considerations are outweighed by the benefits of making an accurate diagnosis and avoiding future morbidity associated with inappropriate treatments." The neurologist is presumably less concerned than other members of the treatment team with the consequences of such an approach because his goal once an accurate diagnosis has been established is to withdraw unnecessary treatment and transfer care to an appropriate psychiatrist.
As it turns out, the differentiation between psychogenic and epileptic seizures has not been as greatly clarified by the use of diagnostic imaging as might be expected. While video EEG, which allows for a comparison of clinical and electrographic features, is considered the gold standard, "caution is required for interpretation" since "failure to see an electrographic seizure does not exclude epilepsy." Thus, while the majority of generalized tonic-clonic seizures show signs of ictal activity on EEG, only 15-33% of simple partial seizures or seizure auras will do so, either because they involve limited brain area or because they are not of superficial origin. In turn, 10-18% of PNES patients will demonstrate intraictal epileptiform abnormalities, despite the fact that they are generally characteristic of epilepsy. A highly specific EEG finding for PNES is "preictal pseudosleep," the clinical appearance of sleep with an EEG that demonstrates wakefulness, although failure to obtain this finding does not rule out PNES. The diagnosis of PNES thus requires a careful comparison of clinical events with EEG changes that may constitute an art as much as a science.
Moreover, there is no single clinical feature that is either sensitive (i.e. a criterion for ruling in) or specific (a criterion for ruling out) for PNES, so that a total clinical picture is required to support the diagnosis. The feature that is described as most characteristic of PNES is the frequent occurrence of episodes in front of a witness, with occurrence in a doctor's waiting room or exam room estimated to have a 75% predictive value for the disorder. Unlike epileptic seizures, psychogenic seizures also do not tend to occur during physiologic sleep (although a phenomenon of xx is considered consistent with PNES), and they are, somewhat surprisingly, less likely to be precipitated by stress or around the time of menstruation. The description of the ictal period in the two disorders is quite distinct. Whereas the ictus of an epileptic seizure is usually brief, lasting less than 1-2 minutes, a psychogenic seizure may last considerably longer, with 78% reporting an episode that qualifies as status epilepticus. While psychogenic seizures are characterized by unresponsive behavior accompanied by motor manifestations that most often mimic either a generalized tonic-clonic or a complex partial seizure, including elements such as tonic posturing and synchronized convulsion (mimicry of atonic, absence or simple partial seizures is considered less common), the patient's eyes are usually open during a generalized tonic-clonic seizure, whereas they may be forced shut during a psychogenic seizure, suggesting the retention of consciousness (in general, incomplete loss of consciousness is considered suggestive of PNES). Whereas motor activity during an epileptic seizure is described as stereotyped, synchronized and progressive, with consistent lateralization, in psychogenic seizures it is more likely to be asynchronous and variable, with a waxing and waning course. Specific movements suggestive of psychogenic seizures include writhing, thrashing, pelvic thrusting, opisthotonus (the famous arched back or arc-en-cercle) and jactitation (rolling from side to side). Vocalization, weeping and icteral stuttering all occur more commonly during psychogenic than epileptic seizures, whereas tongue-biting (especially xx), incontinence and self-injury are more characteristic of epileptic seizures, along with autonomic symptoms such as cyanosis and tachycardia. Finally, the post-ictal period is also distinct: whereas there may be a period of confusion and drowsiness accompanied by headache after an epileptic seizure, headaches are rare following psychogenic seizures, with the patient more likely to reawaken and reorient rapidly and to demonstrate shallow, rapid respirations suggestive of hyperventilation. Interestingly, the symptomatology of PNES is considered most closely related to frontal lobe seizures, although the latter is more likely if seizures are of short duration, they occur during sleep, motor manifestations are stereotyped and the patient's eyes remain open during ictus, whereas a lack of reduction in seizure frequency with antiepileptic drugs or failure to respond to protocols for status epilepticus suggest psychogenic seizure.
We can recognize in this clinical description a number of the key features of Charcot's staging of hysteroepilepsy worked out during the initial nosological phase of his study of hysteria. Although Charcot draws a distinction between an epileptoid phase lasting 1-3 mins. and a clownism phase of similar length that are not differentiated here, the "bizarre posturing" of the hysteric so copiously illustrated in Richer's drawings is clearing recognizable in the writhing, thrashing, pelvic thrusting, opisthotonus and jactitation described as features of the psychogenic ictal phase. The frequent weeping, vocalizations and icteral stuttering that also distinguish PNES correspond to Charcot's emotional phase, in which the patient may display a variety of emotions as well as speaking or crying out. Features of autonomic instability such as incontinence, cyanosis and tachycardia considered more commonly associated with epileptic seizures are not described in hysteroepilepsy. Although the postictal phase is characterized somewhat differently, Charcot speaking of a partial reacquisition of consciousness with a prolonged period of delirium, whereas PNES is thought to have a more rapid postictal reawakening and reorientation, it is emphasized that the latter does not always differentiate the disorder from epilepsy. Friedrich Kittler's observation that "the 'great hysterical arc' can no longer be found in the lecture halls of today's medical schools" (and his concomitant proposal that the invention of hystero-epilepsy should be understood as an effect of filmic technologies that "disappears from nosology or the world shortly after its storage on film") thus seems spectacularly wrong.
If Charcot stumbled in his attempt to provide an etiological explanation for hysteroepilepsy, modern neurology is considerably more circumspect in its willingness to venture an explanation for the disorder's causes. Thus it is only possible to speak of a number of psychiatric disorders that "commonly coexist" with psychogenic seizures, including depression, anxiety, somatoform disorder, borderline or other personality disorders, dissociative disorder, and PTSD. By comparison, schizophrenia and depression with major psychosis are relatively rare associations. 33-50% of patients have a history of physical or sexual abuse, which in the latter case carries with it the risk of a clinically more severe condition that is more likely to resemble epileptic seizures. Dysfunctional family relationships are common. Psychosocial stressors that may precipitate the emergence of PNES include bereavement; unwanted pregnancy; physical, verbal or sexual abuse; lawsuits; financial difficulties; job pressures; impending divorce; domestic conflicts and assault. In children, precipitants include separation anxiety, school avoidance and parental conflicts. A history of neurological insults such as prior head trauma is present in 33-44%, and neurological developmental disabilities are relatively common. Still, the authors warn that it is "impossible to distinguish comorbid from etiologic psychiatric conditions at the present time." Moreover, it is "unproven whether dissociative disorders and somatoform/conversion disorders underlie PNES."
The most provocative hint towards an explanation for the mechanism, if not the etiology, of psychogenic seizures is provided by a recent SPECT study. Demonstrating the continued significance of affective dysregulation in the production of the motor symptoms of conversion, the study demonstrated that conversion disorders may occur when primary motor cortex is overriden by parts of the brain involved in emotion such as the right orbitofrontal and right anterior cingulate cortex.


















